1. What is vitiligo? How does it develop and who is at risk?
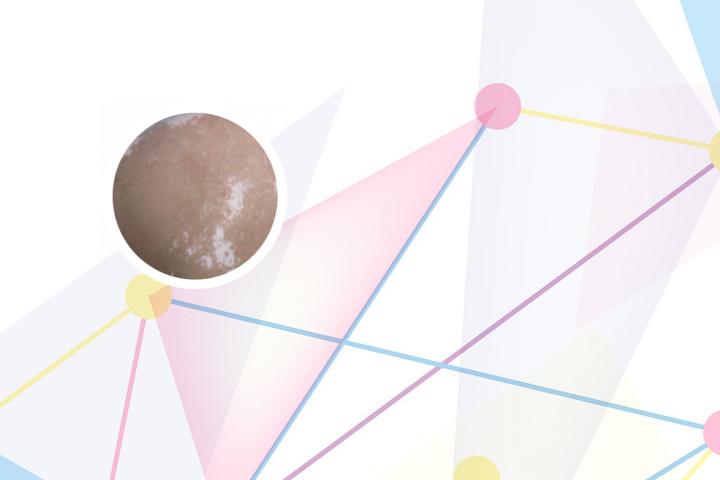
 Vitiligo is a skin disorder characterized by the loss of melanin, which causes white patches on the skin. It occurs due to the destruction or malfunction of melanocytes, the cells responsible for producing melanin. The exact cause of vitiligo is not yet fully understood, but it is believed to be an autoimmune disorder, where the body's immune system attacks and damages the melanocytes. Factors that increase the risk of developing vitiligo include family history, genetic susceptibility, certain autoimmune diseases, viral infections, and exposure to chemicals or toxins.
Vitiligo is a skin disorder characterized by the loss of melanin, which causes white patches on the skin. It occurs due to the destruction or malfunction of melanocytes, the cells responsible for producing melanin. The exact cause of vitiligo is not yet fully understood, but it is believed to be an autoimmune disorder, where the body's immune system attacks and damages the melanocytes. Factors that increase the risk of developing vitiligo include family history, genetic susceptibility, certain autoimmune diseases, viral infections, and exposure to chemicals or toxins.
2. How is vitiligo diagnosed? What are the symptoms?
Vitiligo is typically diagnosed through a physical examination and medical history evaluation. The doctor may also perform a skin biopsy or blood test to rule out other conditions that may cause similar symptoms. The most common symptom of vitiligo is the appearance of white patches on the skin, particularly on the face, hands, feet, and other areas exposed to the sun. The patches may also appear on the eyelids, genitals, and inside the mouth. In some cases, the hair or scalp may also become affected and turn white.
3. What are the treatment options for vitiligo?
The treatment for vitiligo involves a combination of topical and oral medications, UV therapy, and surgical procedures. Topical medications include corticosteroids, tacrolimus, and pimecrolimus creams that can help to stimulate melanocyte growth and reduce inflammation. Oral medications such as psoralen and calcineurin inhibitors may also be prescribed in combination with UV therapy to increase melanin production. Surgical treatments like autologous melanocyte transplantation or punch grafting can be used for patients with stable vitiligo. In addition to medical treatment, camouflage makeup, self-tanners, and tattooing can also help to improve the appearance of the white patches.
4. What are the risks and benefits of treatment options for vitiligo?
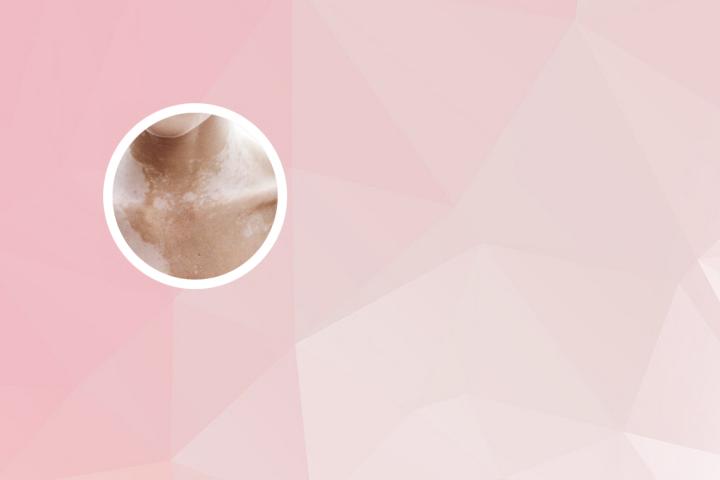
The risks and benefits of treatment options for vitiligo vary depending on the type and severity of the condition, as well as the individual patient's response. Topical medications may cause side effects such as skin irritation, thinning, and discoloration. Oral medications may increase the risk of infection, liver damage, and eye problems. UV therapy can also increase the risk of skin cancer and sunburn. Surgical treatments may have a risk of scarring and infection, but in some cases, they can provide significant improvement in skin pigmentation. The benefits of treatment include improved self-esteem, reduced social anxiety, and better quality of life.
5. How can patients manage their condition and prevent flare-ups?
Patients with vitiligo can manage their condition by adopting healthy skin habits, such as wearing sunscreen, avoiding harsh chemicals or irritants, and moisturizing regularly. Stress management techniques, such as meditation and deep breathing, may also help to prevent flare-ups. Additionally, patients may benefit from counseling or support groups to cope with the emotional impact of living with vitiligo. In some cases, dietary changes or supplements may also be recommended to support overall health and reduce inflammation. It is important for patients to work closely with their healthcare provider to develop a personalized treatment plan and monitor any changes or progression of their condition.